Abstract
Introduction
The use of granulocyte colony-stimulated factor (G-CSF) mobilized peripheral blood stem cells (PBSC) has largely replaced harvested bone marrow (BM) for allogeneic stem cell transplantation. Numerous studies have shown faster neutrophil and platelet engraftment with G-CSF mobilized PBSC, leading to shorter hospitalizations; however PBSC transplantations have been associated to a higher incidence of chronic graft-versus host disease (cGVHD).
Since the late 1990´s, harvested BM of healthy donors has been mobilized with G-CSF. This method increases the number of progenitor cells (CD34+) harvested, which leads to faster engraftment than with unstimulated BM (UBM).
There are no reports comparing the incidence of acute and chronic GVHD with UBM, MBM, and PBSC used to treat diverse benign and malignant hematologic disorders. In this retrospective study, we compare the transplant outcomes of 160 patients from a single institution.
Methods
The charts of patients who received allogeneic HSCT between the February 2011 and September 2016 at our institution were retrospectively reviewed per an IRB approved protocol.
Patients were treated according to current guidelines based on their primary diagnosis and functional status. Donors received Filgrastim (10 mcg/kg/day) for 5 doses prior to harvest. All patients received GVHD prophylaxis with methotrexate (on days +1, 3, 6, 11) and tacrolimus (from day -2 until 4 to 6 months after transplantation).
Statistical analyses were performed using Minitab 17 Statistical Software 2010. A preliminary analysis was completed using Stepwise Regression/ Analyses of variance to determine any relevant covariates. ANOVA and chi-square tests were used to examine group differences in demographic and clinical characteristics or time to engraftment.
Results
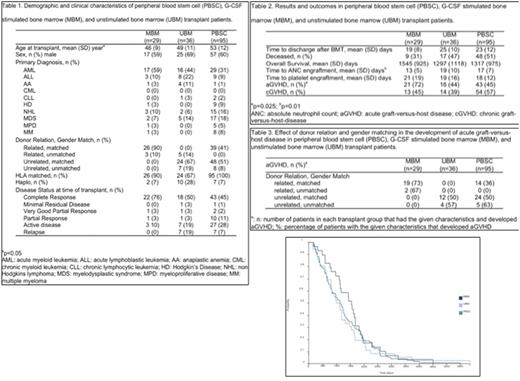
Twenty-nine patients (18.1%) received MBM, 36 received UBM (22.5%), and 95 received PBSC (59.3%). There were no statistically significant differences in patient sex, primary diagnosis, donor characteristics, or disease status between groups. Statically significant differences among groups in patient age were observed (p=0.032, PBSC>UBM>MBM).
Engrafment: MBM was found to have a significantly quicker engraftment of the ANC (13 days), when compared to PBSC (17 days) and UBM (19 days; p=0.01). There were no significant differences in time to engraftment of platelets, between groups.
Acute GVHD: MBM was found to be associated with a significantly higher incidence of aGVHD (72%; p=0.025) versus PBSC (45%) and UBM (44%). Odds ratio's indicate that it may be up to nine times more likely and eight times more likely for MBM to develop aGVHD, when compared to UBM ( 95% CI: 1.15, 9.35)
Chronic GVHD: Patient's treated with PBSC were found to have a higher incidence of cGVHD, when compared to MBM (45%) and UBM (39%); however these findings were not statistically significant (p=0.145) but they showed a trend to significance.
Discussion and conclusion
HLA-matched donors as well as related donors have been associated with lower incidence of GVHD. In our study, 100% of MBM were from related donors, 72% of UBM were from unrelated donors, and 53% of the PBSC donors were unrelated. There was a higher incidence of acute and chronic GVHD in MBM, even though they were from HLA-matched related donors; the results were statistically significant for aGVHD and there was a clear trend on cGVHD. Additionally, despite having increased incidence of acute and chronic GVHD, patients who received MBM had better overall survival; this is likely secondary to graft versus leukemia. The main limitations of the study are the sample size and that it is possible that some of the patients have not developed cGVHD yet, therefore it is necessary to obtain data from a larger cohort and with a longer follow up, additionally, since this is a retrospective study access to grade and stage of GVHD is limited for some patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.